Appearing On:














Serious injuries deserve experienced attorneys
 DC Injury Lawyers
DC Injury Lawyers
A personal injury case is a civil action, which means that if have suffered an injury to yourself and a person or a business is found legally responsible for causing your injuries, the remedy comes in damages, which is money awarded to you and paid by the liable party (the defendant) to the injured party (the plaintiff). Settlements and court awards in personal injury cases typically range from $3,000 to $75,000. But many factors can affect these numbers, which is why contacting a personal injury law firm in Washington DC is so important. A “tort” is a wrongful act or an infringement of a right (other than under contract) leading to civil legal liability. The four elements of tort law are duty, breach of duty, causation, and injury. In order to claim damages, a defendant must breach the duty toward the plaintiff, which results in an injury. There are three main types of torts, which are negligence, strict liability (product liability), and intentional torts. When selecting a firm, you may also want to check out our Google reviews, left by hundreds of our clients. You have to find out more about our reputation here: Whether another person, company or large corporation is at fault, we won’t let anyone bully you out of the compensation you deserve. Our founding partner, Wayne Cohen, is regularly appearing in the press. He discussed courtroom lawyers’ use of AI on CNBC, How Law Firms Are Using Artificial Intelligence in Their Practices on US News, Holiday Injuries on Newsweek and more.
Our top-notch, Washington DC personal injury lawyer team is comprised of caring, compassionate, and dedicated men and women who have made it their life’s work to fight tirelessly for your rights.
Understanding Personal Injury Law in Washington, D.C.
Navigating the aftermath of a personal injury in Washington, D.C., can be overwhelming. The physical pain, emotional distress, and financial burdens often leave victims feeling lost. In these challenging times, we step in to provide the guidance and support you need. Our comprehensive approach ensures that your rights are protected, and you can pursue rightful compensation while focusing on your recovery.
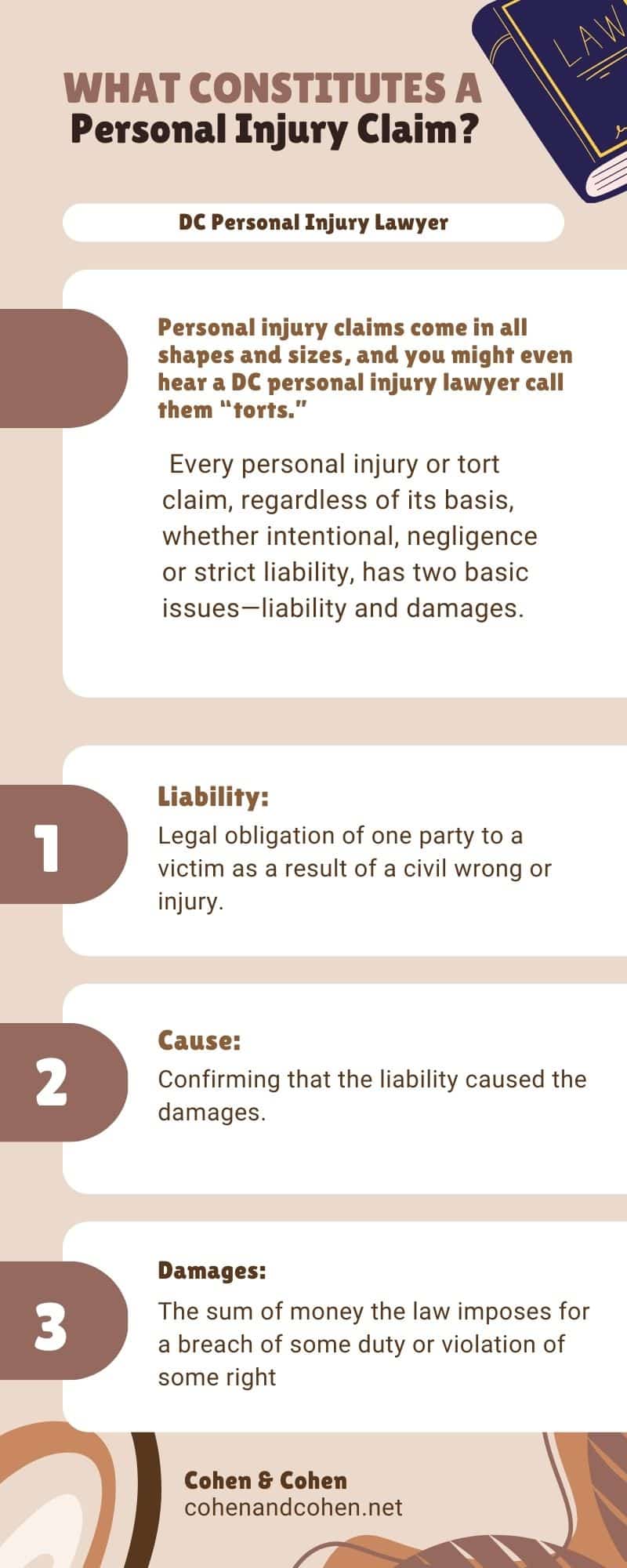
Personal injury claims come in all shapes and sizes, and you might even hear a DC personal injury lawyer call them “torts.” Every personal injury or tort claim, regardless of its basis, whether intentional, negligent, or strict liability has two basic issues—liability and damages.
- Liability: Legal obligation of one party to a victim as a result of a civil wrong or injury.
- Cause: Confirming that the liability caused the damages.
- Damages: The sum of money the law imposes for a breach of some duty or violation of some right.
- Compensatory Damages: Money paid to compensate the injured party based on his or her loss or injury.
- Punitive damages: Money paid to the victim as a punishment to the wrongdoer (used for intentional torts typically).
Essentially, any personal injury lawyers Washington DC has to offer will know that a personal injury claim has to answer the following questions: was the defendant (company, employer, wrongdoer, etc.) liable for the sustained damages? If so, what is the extent and nature of the damages? A good DC personal injury lawyer will be able to listen to your concerns, empathize with the situation the wrongdoer has put you in, and be able to determine the fair and just compensation you deserve to get you back on your feet.
Personal injury law, or tort law, addresses situations where someone’s negligence or intentional actions cause harm to another. In Washington, D.C., this includes a range of incidents such as:
- Car Accidents: Collisions involving cars, motorcycles, trucks, and pedestrians.
- Slip and Fall Incidents: Injuries caused by hazardous conditions on properties.
- Medical Malpractice: Harm resulting from negligence by healthcare professionals.
- Product Liability: Injuries caused by defective or dangerous products.
- Workplace Accidents: Injuries occurring during employment.
Victims in D.C. have the right to seek compensation for medical expenses, lost wages, pain and suffering, and other damages.
How We Help as Personal Injury Lawyers in D.C.
We take pride in serving as advocates for injury victims, guiding you through the complexities of personal injury law. Here’s how we support you:
- Case Evaluation: We assess your claim to determine its viability and potential outcomes.
- Evidence Collection: Our team gathers medical records, accident reports, witness statements, and other vital information.
- Negotiation: We handle discussions with insurance companies to secure fair settlements.
- Litigation: If necessary, we represent you in court to fight for justice.
- Legal Guidance: We keep you informed every step of the way, explaining your rights and options clearly.
Why Work With Us in Washington, D.C.?
As local attorneys, we bring unique advantages to your case:
- In-Depth Knowledge: We’re well-versed in D.C.’s specific laws and regulations.
- Familiarity with Local Courts: Our understanding of local court procedures and personnel benefits your case.
- Local Resources: We have access to trusted investigators, medical professionals, and other experts in the area.
Steps You Should Take After a Personal Injury in D.C.
If you’ve been injured, taking these steps can help protect your rights and strengthen your case:
- Seek Medical Attention: Always prioritize your health by consulting a medical professional, even if injuries seem minor.
- Document the Incident: Take photos, gather witness contacts, and keep detailed notes about the incident.
- Report the Incident: Notify the appropriate authorities or property owners to create an official record.
- Consult Us: The sooner you speak with us, the better we can preserve evidence and explore your legal options.
- Avoid Public Discussion: Refrain from sharing details on social media or with unauthorized parties.
Understanding Deadlines in Washington, D.C.
It’s crucial to act quickly, as personal injury claims in D.C. are subject to strict deadlines:
- General Personal Injury: Typically three years from the date of injury.
- Medical Malpractice: Generally three years from the injury or one year from discovery.
- Wrongful Death: Usually one year from the date of death.
We can help confirm the specific deadlines for your case.
DC Personal Injury Law Infographics
Compensation You May Be Entitled To
We work to secure the maximum compensation available, which can include:
- Economic Damages: Medical bills, lost wages, rehabilitation costs, and property damage.
- Non-Economic Damages: Pain and suffering, emotional distress, and loss of enjoyment of life.
- Punitive Damages: In cases of egregious conduct, additional damages to hold the wrongdoer accountable.
Choosing the Right Lawyer Matters
When selecting an attorney, you deserve a team that delivers results. Here’s what to look for:
- Experience: A proven track record in personal injury cases.
- Reputation: Client testimonials and peer reviews that highlight success.
- Resources: The capability to handle complex cases effectively.
- Clear Communication: Regular updates and a transparent approach.
Overcoming Challenges in Personal Injury Cases
We understand the obstacles you may face, such as:
- Insurance Company Tactics: Insurers may try to minimize or deny claims.
- Proving Liability: Establishing fault can be tricky, especially with multiple parties involved.
- Calculating Damages: Quantifying non-economic damages requires skill and experience.
Tips for Picking a Washington DC Personal Injury Lawyer:
- Do your research: Not every personal injury law firm has your best interest at heart. Many are just looking to make a quick buck off of your case. This often leads to you getting paid far less than you and your loved ones deserve. Instead, find a DC personal injury attorney who listens to you; cares about your story, and is dedicated to keeping you informed during every step of the process.
- Look for a firm with a long history in the community or jurisdiction: Firms like these know their stuff. They attract the kind of personal injury lawyer Washington DC residents deserve. Their clout in the community, their relationship with the court, and their understanding of the unique circumstances that affect Washington DC and Metro area residents is an unbeatable combination and will yield the highest personal injury payouts.
- Look at their awards and accolades: The legal community acknowledges excellence and achievements through a variety of awards and publications. Look for firms that have a long list of top performances, impressive verdict/settlement payouts, and recognized personal injury attorneys.
DC Personal Injury Law Statistics
Washington D.C is known for its high volume of traffic, and thus the city has a relatively high rate of motor vehicle accidents compared to other cities. The high population density and high rate of the vehicle and pedestrian accidents often lead to personal injury claims. Additionally, the city’s large number of tourists and visitors may also contribute to the number of accidents in the city. Motor vehicle injuries are the second-highest cause of fatalities with 12.4 people per 100,000 population each year in the US. According to the National Highway Traffic Safety Administration (NHTSA), last year there were an estimated 38,800 deaths resulting from motor vehicle crashes. Additionally, there were an estimated 4.4 million people injured in motor vehicle crashes that same year. There are many factors that contribute to the high number of car accidents in the US, including distracted driving, drunk driving, speeding, and poor road conditions. Efforts to reduce the number of car accidents in the US include increased enforcement of traffic laws, public education campaigns, and improvements in vehicle safety technology.
DC Personal Injury Lawyer FAQs
When you’ve been unexpectedly injured due to the negligence of another person, it’s a good idea to find out what a personal injury lawyer Washington DC trusts has to say. At Cohen & Cohen, we understand you may have a lot of questions about what your legal options may be. As a well-respected DC law firm, we aim to help our clients navigate the legal system in effective ways. Through aggressive representation and decades of experience, we work tirelessly to get clients maximum compensation. To discuss your case with a Washington DC personal injury lawyer now, please call Cohen & Cohen
- What Is The Value Of My Case?
- What should I do if I’ve been in a car accident?
- How has tort reform changed my ability to make a claim?
- Personal Injury Lawsuit FAQs
- Personal Injury Claims FAQs
- Damages from Personal Injury Accidents
After a personal injury, you may have several questions about what steps to take in order to safeguard your personal and financial well-being. It is our objective to provide you with helpful information to move forward. Some of the most common questions we get from clients, and their respective answers, are as follows:
Who can be held liable?
To determine accurate liability, a personal injury lawyer in Washington DC should investigate all available pieces of evidence. There could be more than one party responsible for your injury and may include an employer, doctor, drug manufacturer, driver of another vehicle, hospital, and so forth.
Should I sign anything?
Prior to making any oral or written agreements you should contact a personal injury lawyer Washington DC depends on for sound legal advice. By signing a document, such as a release, you may put yourself at risk of being unable to recover damages. A capable law firm, such as Cohen & Cohen may help to ensure that your rights are fully protected and that you don’t get anything less than what you deserve.
I am partially at fault for my personal injuries. Can I still pursue a claim?
This particular situation will be dependent upon your local jurisdiction and state. Sometimes, when partial negligence is involved, a claim is not pursuable. However, most areas maintain the ability for victims to still file a claim for compensation, which could be decreased in accordance with the victim’s degree of carelessness.
What will a lawyer cost me?
At Cohen & Cohen, we take personal injury claims based on contingency. This means you are not required to pay anything upfront. Instead, you would only pay if and when the case results in a settlement.
How soon should I file a legal claim?
Realistically you should speak with a personal injury lawyer in Washington DC offers as soon as possible. Personal injury claims must be filed within a certain time period. Failing to meet this deadline can restrict your ability to recover monetary damages.
How much is my case worth?
It’s impossible to say how much a case is worth without actually speaking to a personal injury lawyer Washington DC relies on. The worth of your claim may depend on the extent of your injuries, the underlying factors, insurance limits, the defendant, and more. A straightforward claim may enable you to receive compensation for:
- Past, ongoing, and future medical bills
- Lost wages
- Loss of earning capacity
- Pain and suffering
- Emotional anguish
- Punitive damages (when applicable)
What Damages Can You Recover After an Injury Accident?
If you want some of the best personal injury lawyers Washington DC may offer, contact us at Cohen & Cohen immediately. If you’ve been seriously injured through no fault of your own, you may wish to seek legal advice without delay. Medical bills can add up very quickly and you may also be missing work during your recovery. Don’t wait to get a lawyer to fight for your rights. As one of the best personal injury attorneys in Washington DC, Wayne Cohen may help you recover damages from the responsible party. Call our DC office at (202) 955-4529 to schedule a free consultation. For now, here is an answer to one of the most common questions we hear from personal injury victims.
Cohen & Cohen DC Personal Injury Attorney
1730 Rhode Island Avenue, NW Suite #410 Washington, D.C. 20036
DC Personal Injury Attorney Google Reviews
“My experience with Cohen and Cohen surpassed my expectations. Since the first day that I called, I was helped. Great customer service overall and every single person that I spoke to was amazing. The team at Cohen and Cohen was very understanding and kept me in the loop with what was going on with my case. Today my case was closed and I’m happy with the outcome. Thank you all for everything. Thank you for all your hard work. 10 stars!” – Atiuq N.
Our DC Personal Injury Attorney Team Can Help!
Don’t let yourself or your loved ones get bullied out of the compensation you deserve. Cohen & Cohen is a firm dedicated to making sure your rights are looked after. From beginning to end, our skilled team will work with you to make sure you understand every step of the litigation process. We empathize with the pain and suffering you’re going through and will work tirelessly to make sure that every ounce of evidence proving your case makes its way in front of the court, so the right verdict or settlement is awarded. Don’t settle for just any DC personal injury attorney. Your life and livelihood are more important than that. You deserve to have someone experienced and passionate fighting in your corner. The top-notch personal injury lawyer Washington DC deserves is just a phone call away; contact us.
Acting Quickly Is Essential
Timely action can make a significant difference in your case:
- Preserve Evidence: Collecting evidence early strengthens your claim.
- Witness Accuracy: Statements gathered promptly are more reliable.
- Meet Deadlines: Filing within the statute of limitations is critical.
Choose Cohen & Cohen
If you’ve landed on this page, odds are you or a loved one has suffered a catastrophic personal injury, and you need help from a personal injury lawyer DC residents have turned to for decades. The decision you make in selecting the right lawyer for your case is imperative, and we encourage you to do your homework before selecting a personal injury attorney. Here are 5 things to know about our firm:
- Wayne Cohen, our founding partner, began the practice of law in 1991 and founded the firm in 1993. Wayne was born in Washington, D.C., and raised in the Washington Metropolitan area. A former boxer, Wayne understands how important it is for clients of the firm to understand that they are incompetent hands when they have a personal injury case.
- Together with his partners Jill Stanley, Adam Leighton, and Kim Brooks Rodney, Wayne, and the team have had appearances on ABC, NBC, CBS, the Today Show, Good Morning America, CNN, USA Today, the Washington Post, Jet Magazine, the Boston Globe, the LA Times, and many, many more. For decades so many man members of the press have sought comment about the firm’s cases, and other cases, and have turned to the competence of the personal injury lawyers at the firm.
- The firm is very, very proud of its reviews. Like you, each of our clients began the scary process of finding a lawyer by turning to the internet. Take a minute, and Google the phrase: “Cohen and Cohen Washington dc” and, as of April 10, 2022, you’ll see hundreds of reviews.
- Wayne Cohen and Kim Brooks Rodney have been identified by Washingtonian Magazine as two of the top personal injury lawyers in this area over, and over, and over again. They have regularly been called “the best” and “the top” repeatedly.
- Partner Kim Brooks Rodney worked for the insurance industry for roughly two decades, before changing sides and fighting for the rights of injured victims. Ask yourself, if you’re fighting against an insurance company (almost all cases have insurance), don’t you want a law that truly understands how to get the most compensation from insurance companies as quickly as possible?
Let Us Help You Move Forward
Suffering a personal injury in Washington, D.C., is life-altering, but you don’t have to face it alone. We’re here to guide you through the legal system, protect your rights, and pursue the compensation you deserve. By taking proactive steps and relying on our dedicated support, you can focus on healing while we handle the rest.
Personal Injury Attorneys In:
Washington DC | Maryland | Virginia
“Cohen & Cohen did a great job at recovering a good amount of money for me after my accident. Siri was super informative & responsive. Overall I had a great experience using this firm & they will be my first call if I am ever in an accident again.”
– Charles M.
 Personal Injury Accident
Personal Injury Accident
“I had a very positive experience with Cohen & Cohen and I highly recommend them to anyone who needs their services.”
– John G.
 Tractor Trailer vs Car
Tractor Trailer vs Car
“I would highly recommend Cohen & Cohen. They were awesome on my case. Cohen & Cohen had my best interest at heart at all times.”
– Morgan L.
 Personal Injury Accident
Personal Injury Accident
“My experience at Cohen & Cohen has been great from the beginning until the very end when my case was closed…I would definitely recommend them to family, friends or anyone that has a case with a personal injury accident.”
– Maria M.
Reviews
From Our Valued Clients
Cohen & Cohen has an impeccable client satisfaction rating with hundreds of 5-star reviews. We are among the best-rated firms in D.C., Virginia, and Maryland.

Best Personal Injury Lawyer in DC








Cohen & Cohen Has Been Featured On